Plantar fasciitis is a common foot condition characterized by sharp, stabbing pain in the heel, typically felt most acutely with the first steps in the morning. This discomfort is caused by inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. Often developing without an obvious cause, plantar fasciitis can be a lingering source of frustration for those affected, impacting daily activities and quality of life.

Misdiagnosis can sometimes occur due to the overlap of symptoms with other foot conditions. Not all heel pain is attributable to plantar fasciitis; therefore, it’s vital to consider other potential causes such as Achilles tendinitis, heel spurs, or tarsal tunnel syndrome. Accurate diagnosis typically involves a physical examination, consideration of the individual’s medical history, and sometimes imaging tests to rule out other concerns.
Managing plantar fasciitis usually entails a combination of rest, ice, and stretching exercises, along with possible interventions such as orthotics, physical therapy, or anti-inflammatory medications. Conservative treatments are effective for many, though persistent cases may require more advanced methods, including corticosteroid injections or surgery. Prevention strategies like wearing supportive shoes and maintaining a healthy weight can also help mitigate the risk of developing plantar fasciitis.
Understanding Plantar Fasciitis
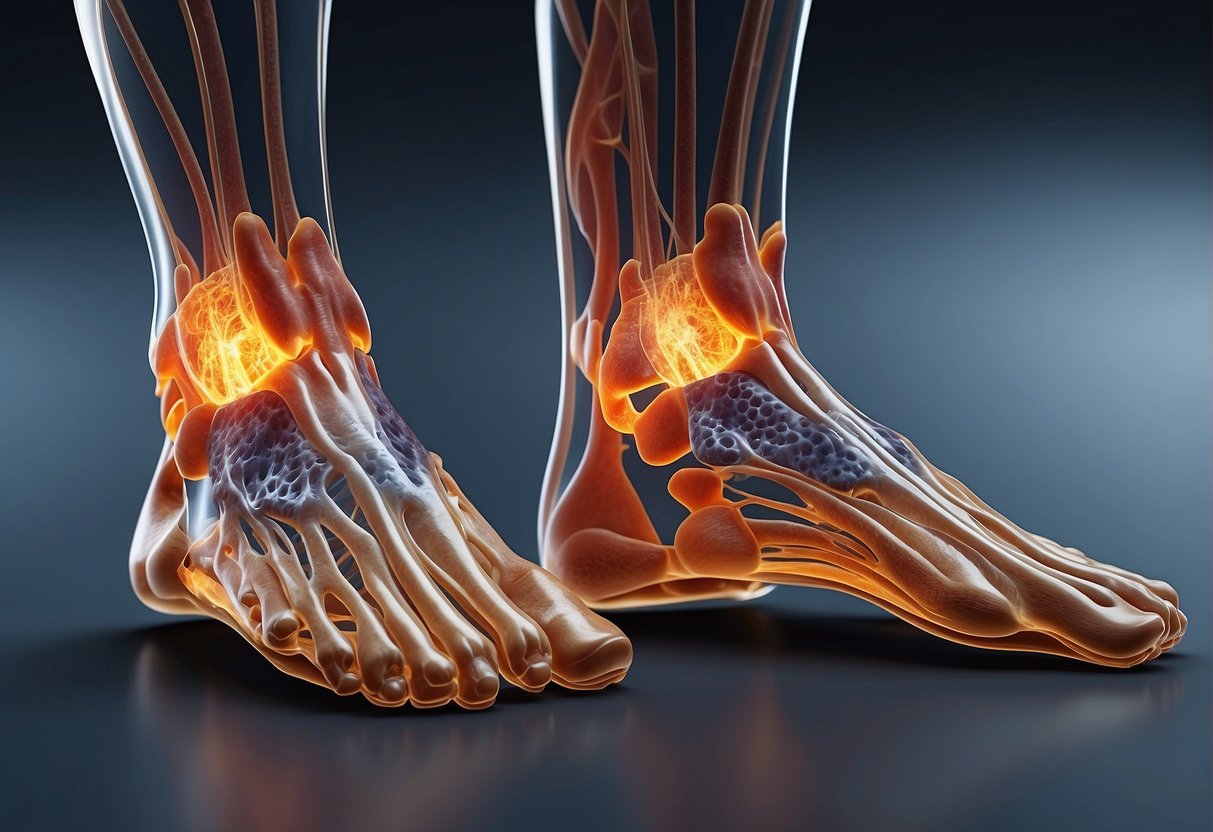
In addressing plantar fasciitis, it is crucial to comprehend the foot’s anatomy and how the condition manifests through inflammation and microtears in the tissue.
Anatomy of the Foot
The plantar fascia is a thick band of tissue that runs across the bottom of the foot, connecting the heel bone to the toes and supporting the arch of the foot. This structure is integral to the foot’s ability to bear weight and absorb impact.
What Is Plantar Fasciitis?
Plantar fasciitis refers to the inflammation of the plantar fascia. This condition often results from strain and stress leading to small tears in the fascia. When the tissue is overloaded or overstretched, it can become swollen, weak, and irritated, causing pain in the heel or bottom of the foot.
Causes and Risk Factors

Plantar fasciitis stems from various causes and is influenced by several risk factors that can increase individual susceptibility to the condition.
Biomechanical Issues
Flat feet and high arches are structural foot conditions that can contribute to plantar fasciitis. They can lead to an imbalance in foot mechanics, affecting how weight is distributed when a person stands or moves. A flat arch can cause the plantar fascia to stretch excessively, while a high arch can lead to an inadequate shock absorption. Both scenarios place additional stress on the plantar fascia.
Lifestyle and Activities
Individuals who are overweight or obese may experience added pressure on the plantar fascia due to the excess weight they carry. This increased load can significantly contribute to the development of plantar fasciitis.
Regular participation in activities that put stress on the heel—such as long-distance running, ballet dancing, aerobic dance, or occupations that require extended periods of walking or standing—can wear the plantar fascia and cause inflammation, especially when these activities are done without proper footwear or with inadequate rest.
| Risk Factor | Description |
|---|---|
| Exercise | High-impact activities like running and jumping may lead to overuse and strain on the plantar fascia. |
| Standing | Prolonged periods on feet, especially on hard surfaces, without breaks can exacerbate the stress on the heel. |
| Walking | Excessive walking, particularly in unsupportive footwear, can harm foot mechanics and contribute to plantar fasciitis. |
| Age | Plantar fasciitis is more common in individuals aged 40 to 60. |
| Occupation | Jobs that require a lot of walking or standing can increase the risk of developing plantar fasciitis. |
Management of lifestyle factors and awareness of individual biomechanical issues can help mitigate the risk of developing plantar fasciitis.
Diagnosis and Evaluation

Accurate diagnosis of plantar fasciitis involves a detailed evaluation by a healthcare professional. This typically includes a thorough physical exam and may also involve imaging techniques to rule out other conditions.
Physical Exam
During the physical exam, a doctor looks for tenderness on the bottom of the foot, specifically the area of the heel where the plantar fascia attaches to the bone. They will assess the foot’s arch and the strength and health of the muscles. Flexibility tests to evaluate the Achilles tendon and plantar fascia tightness are common, as tight tendons can contribute to plantar fasciitis.
Imaging Techniques
- X-ray: While an x-ray will not show the plantar fascia, it can reveal if a bone spur is present, which may be associated with the pain.
- MRI: Magnetic Resonance Imaging (MRI) is not typically ordered but may be used if the diagnosis is uncertain or if symptoms persist despite appropriate treatment. MRI can provide detailed images of the plantar fascia and identify other possible causes of heel pain.
Treatment Options

Individuals facing plantar fasciitis have a variety of treatment options ranging from conservative measures to more advanced therapies. It is important to select a treatment plan that aligns with the individual’s specific condition severity and lifestyle needs.
Conservative Treatments
For those recently diagnosed or experiencing mild symptoms, the following conservative treatments are often recommended:
- Rest and Ice: Decreasing or momentarily stopping activities that exacerbate pain is suggested. Applying ice to the affected area can reduce inflammation.
- Stretches and Physical Therapy: Regular stretching exercises, such as calf stretches and plantar fascia-specific stretches, can alleviate tension. Physical therapy may improve flexibility and strengthen foot muscles.
- Supportive Shoes and Orthotics: Wearing shoes with proper arch support and cushioning helps distribute pressure evenly. Over-the-counter or custom orthotics can further enhance this support.
- Night Splints: These devices maintain the ankle in a dorsiflexed position overnight to stretch the plantar fascia gently.
Implementing these treatments can help manage symptoms effectively.
Advanced Therapies
If conservative treatments are not successful, the following advanced therapies may be considered:
- Steroid Injections: These can provide temporary relief from inflammation and pain but should be used sparingly due to potential side effects.
- Platelet-Rich Plasma (PRP) Injections: Utilizing the patient’s own blood components to promote healing, PRP injections are a newer treatment modality gaining popularity.
- Extracorporeal Shock Wave Therapy (ESWT): This noninvasive procedure uses sound waves to stimulate healing in the plantar fascia.
- Surgery: As a last resort, surgical release of the plantar fascia may be considered when other treatments fail to provide relief.
Advanced therapies are often used in combination with continued conservative treatment methods to support the arch and regain full functionality.
Prevention and Management
Effective management and prevention of plantar fasciitis involve consistent effort in adapting lifestyle choices and integrating specific exercises. These strategies can significantly reduce the risk of developing symptoms and aid in managing discomfort if the condition is already present.
Lifestyle Adjustments
Individuals should consider weight management as a crucial factor in preventing plantar fasciitis, as carrying extra weight can put additional stress on the plantar fascia. Shoes play an essential role; it’s advisable to wear supportive footwear that fits well and offers proper arch support. Making activity modifications to avoid excessive strain can also be beneficial. This entails avoiding prolonged periods of standing and opting for activities that are low-impact on the feet.
Exercise and Stretching
Incorporating specific exercises and stretching routines into daily life can help manage and prevent the stiffness associated with plantar fasciitis. Here are recommended exercises:
- Calf Stretches: To prevent tightness in the posterior leg muscles that can affect the plantar fascia.
- Gastrocnemius Stretch: Stand arm’s length from a wall, step one foot back, keep it straight and heel down, then lean forward until a stretch is felt.
- Plantar Fascia Stretch: This stretch targets the plantar fascia directly.
- Sit down and cross one leg over the other. Use your hand to pull the toes back towards your shin until you feel a stretch along the arch of your foot.
A routine that includes a combination of these stretches should be performed regularly to help maintain flexibility in the muscles that are interconnected with the plantar fascia, thus aiding in both treatment and prevention of injury.




